Stress ulcers are a common condition that can affect anyone, but are most commonly found in people with chronic illnesses and those who have to work in high-stress environments. Stress ulcer prevention is essential for protecting against these types of digestive issues.
Table of Contents
What are stress ulcers?

Photo by Sora Shimazaki from Pexels
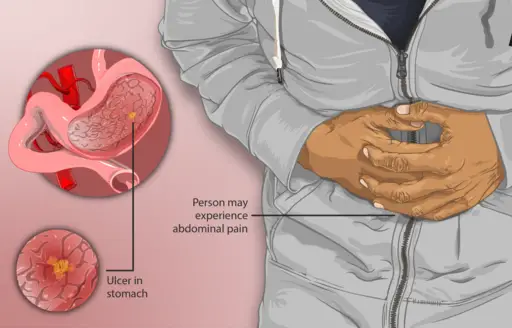
Usually occurring in the fundus and body of the stomach, stress ulcers are characterized by numerous superficial erosions. As a result of shock, sepsis, and major trauma, they often develop in patients with peritonitis and other chronic illnesses.
A stress ulcer is not the same as a peptic ulcer. A peptic ulcer is made worse by stress, but a stress ulcer is not.
Some people have stomach ulcer, also called gastric ulcer. There are two types of ulcers – peptic ulcers and stress ulcers. The difference between the two is that a peptic ulcer happens gradually while a stress ulcer happens suddenly.
Some foods can make your ulcer worse. Physical or physiologic stress like a severe injury or infection can also make it worse. This may be because stress makes the stomach make more acid.
Stress ulcers are life-threatening but not as much as stomach ulcers. Furthermore, it is important to distinguish stress ulcers from reactivation of chronic duodenal ulcer or gastric ulcer.
Causes of Stress Ulcers
The stomach makes acid to help digest food. If your stomach is too acidic, then you might get an ulcer.
Under severe physiological stress, ulcers may occur because the acid in your body changes. For example, a Helicobacter pylori (H. pylori) infection makes you more likely to get all ulcers. A stress ulcer is one of those.
A stress ulcer is rarely caused by psychological stress.
Certain factors in your health and lifestyle can cause damage to your stomach lining. In addition, some factors make it more likely for someone to have an ulcer. These include stress-related ulcer, a family history of ulcers, stomach acids that are too strong, and a person’s diet. In addition, H. pylori and nonsteroidal anti inflammatory drug (NSAID) can also cause ulcers.
If you have had a health emergency or injury and have had ulcers in the past, you are more likely to get a stress ulcer.
Stress can cause a person’s stomach to hurt. Foods may make the pain better or worse. A person with a stress ulcer is already sick, so it can be hard to tell if they have an ulcer or another illness.
 Stress ulcer can cause several symptoms, including abdominal pain that improves or worsens with food; unusually bloated feeling; vomiting or nausea and shortness of breath. Stress ulcer also affects your skin and causes anemia-related symptoms like pale skin these are the signs you should watch for if stress ulcer is becoming too much to handle on its own.
Stress ulcer can cause several symptoms, including abdominal pain that improves or worsens with food; unusually bloated feeling; vomiting or nausea and shortness of breath. Stress ulcer also affects your skin and causes anemia-related symptoms like pale skin these are the signs you should watch for if stress ulcer is becoming too much to handle on its own.
What is the worst thing about ulcers? Not just being in pain, but it can also make you bleed a lot. This upper gastrointestinal bleeding may be dangerous for those who have serious injuries, like head injuries, because they might die when their blood loss exceeds what they need to stay alive.
Symptoms of a rapidly bleeding ulcer include excessive vomiting, diarrhea or blood in the stool. Other symptoms are red vomit, fainting, fever and unusual tenderness of the stomach.
It is important to know the signs of a rapidly ulcer bleeding so you can avoid it happening again or getting worse. Keep your doctor informed on any new symptoms that may happen because they are necessary for prevention. If this doesn’t work, then emergency care needs to be sought out.
Stress Ulcer Prophylaxis (SUP) – Prevention
Stress ulcer prophylaxis is routinely prescribed to severely ill patients to safeguard against clinically critical ulcer bleeding from the upper gastrointestinal tract.
SUP is vital because it helps prevent the recurrence of a stress ulcer and lessens the severity if a new one develops, reduces hospitalization time, and improves nutritional status, which can reduce morbidity and mortality rates.
Stress ulcer prophylaxis is a preventative measure in critical care medicine that has been shown to minimize the rate of stress ulcer development and reduce the incidence of stress-induced ulcers. In addition, stress-related acid secretion and gastric emptying may be reduced by medications such as H-blockers, proton pump inhibitor, antacids, or sucralfate.
Research suggests that Histamine-2 receptor antagonists (Histamine-2 receptor blockers: H2 blockers) are the most efficient in reducing bleeding in critical care patients and do not increase hospital-acquired pneumonia, while mortality rates remain unchanged.
Histamine 2 receptor blocker is the most commonly prescribed medication for gastric ulcers. They help to decrease stomach acid secretion and reduce the risk of ulcers. These medications include cimetidine, famotidine (Pepcid), nizatidine (Axid) and ranitidine hydrochloride (Zantac).
Proton pump inhibitor (PPI) is also used in preventing stress ulcers in intensive care patients.
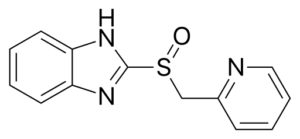 The basic idea is that these medications inhibit stomach acid production, which means less of the “bad” kind of hydrochloric acid in your gut. It’s also worth noting that proton pump inhibitors are not a cure for stress ulcers – they’re more like prevention pills.
The basic idea is that these medications inhibit stomach acid production, which means less of the “bad” kind of hydrochloric acid in your gut. It’s also worth noting that proton pump inhibitors are not a cure for stress ulcers – they’re more like prevention pills.
PPIs are better at keeping your stomach in an alkaline environment than H2 receptor antagonists. This is because PPIs can work at a lower pH than H-antagonists.
The correct dosage of PPI for prevention should be given as soon as possible after the patient has entered intensive care and continued until hospital discharge. The duration depends on how long they’re in intensive care units (ICUs), ranging from a few days to weeks. It’s important to note that PPIs cannot be given for more than one year without a break because of the risk of developing kidney and bone problems.
In addition to their beneficial effects on gastric mucosal blood flow, PPIs may also exhibit antioxidant effects. This results from a new study that found their use may help protect against damage from free radicals. Free radical-caused tissue damage can lead to ulcers, and some experts believe PPIs are an effective prevention measure for this reason.The safety of proton pump inhibitor are well described.
PPI prophylaxis has also been shown to be beneficial in preventing stress ulcer recurrence.
Inhibitors versus histamine: Though it is considered by many to be the best prophylactic treatment to prevent rebleeding in stress ulcers, there is not enough evidence to support its routine use (instead of H2 antagonists) for preventing stress ulcers. However, in the rare event that a person has had two ulcers or more within five years and is at risk of rebleeding, proton pump inhibitor may be considered.
The third group of possible SUPs would be antacids and sucralfate. These are both in the same family of medications that work by binding to and neutralizing acid. Sucralfate should not be taken with medications that reduce stomach acids, such as antacids or H-blockers.
Sucralfate is a good choice for adult patients who cannot take PPIs because of the risk of heartburn and gastroesophageal reflux disease (GERD). It can also help protect ulcers from infection by coating them (similarly to how an antibiotic would).
Stress ulceration occurs in a small minority of patients, and it continues to decrease with time, which means that routinely prescribing prophylaxis for all patients at risk is probably not cost-effective.
Furthermore, the evidence that has been accumulated suggests patients without mechanical ventilation, those with no coagulopathy (a condition in which the blood can’t form clots), those on enteral nutrition and those who do not have a significant organ failure do not need prophylaxis.
Stress ulcer: Diagnosis and Treatment
A diagnosis of a stress ulcer is based on the patient’s history and physical examination. Upper gastrointestinal endoscopy with biopsies may also be necessary to confirm the diagnosis in some cases. However, it does not provide therapeutic benefit for treatment because no medications specifically target these types of lesions.
Stress ulcers can require surgical procedures when the ulcer is not healing or there are complications, such as perforation of the gastric wall or renal failure.
During an upper gastrointestinal endoscopy with biopsies, a gastroenterologist will take small tissue samples from the stomach and duodenum lining to examine under a microscope for erosion caused by stress.
Management of a stress ulcer follows the same principles as for a chronic ulcer and resembles the management of erosive gastritis.
In some cases, endoscopic treatment of stress ulcers may be ineffective, so an operation is required since the blood is shunted away from the mucosa, making it more vulnerable to damage.
A preventative approach is usually the first step in treating stress ulcers. Particular attention should be paid to respiratory status, acid-base balance, and treatment of other critical illness that can contribute to stress ulcers.
Although patients with stress ulcers do not secrete large quantities of gastric acid, the acid does appear to be a factor in developing the disease (i.e., pathogenesis). For this reason, it may be appropriate to either neutralize or inhibit the secretion of gastric acid when a patient is at high risk of stress ulcer.
Those with active bleeding (especially in the stomach due to ulcers) or other GI disorders which may cause ulcers should be administered an antacid and H2-blocker mixture. Those who have gastritis or ulcerations can receive a selective injection of vasopressin into the left stomach artery for help in controlling bleeds.
Does stress cause ulcers?
 According to research, psychological stress alone is not to blame for peptic ulcers. But we know that when the body is under stress, such as when a person is sick, the body’s healing ability is impaired. That means that a person’s body is less able to heal from an ulcer and will be more likely to get another one. So, stress alone may not cause an ulcer, but it does impair the healing of existing ones. Other ulcers, such as mouth ulcers and peptic ulcers, may not be directly caused by stress
According to research, psychological stress alone is not to blame for peptic ulcers. But we know that when the body is under stress, such as when a person is sick, the body’s healing ability is impaired. That means that a person’s body is less able to heal from an ulcer and will be more likely to get another one. So, stress alone may not cause an ulcer, but it does impair the healing of existing ones. Other ulcers, such as mouth ulcers and peptic ulcers, may not be directly caused by stress
Stress-related conditions like chronic anxiety or depression can lead to stomach problems, including peptic ulcer disease, because they can lead to other illnesses or make an existing illness worse.
Smoking cigarettes or overindulging in large amounts of alcohol are two examples of stressors that may increase the risk for stomach ulcers. Besides damaging a body’s ability to heal, these habits can cause ulcers and aggravate current symptoms.
When someone suffers from other illnesses, such as an autoimmune disorder or some viral infections, they might develop ulcers.
Unexpected results can occur when we suffer from stress. Ulcers are not directly related to it, but most of us do have ulcers, and they need to be controlled because long-term stress will only lead to poorer health, which nobody wants. Prevention of stres and stress management may help reduce symptoms such as heartburn or reflux in some people with a history of stomach ulcer.
One more connection between stress and ulcers has to do with the stress caused by ulcer formation.
Having mouth ulcer can be a very stressful experience and may even cause anxiety due to the pain and the way it affects your ability to talk, chew, eat, and drink.
You might already be dealing with a sense of stress due to work related pressure, for example, but mouth ulcer can contribute to it even more.
Conclusion
There are a lot of misconceptions about stress ulcers. A common misconception is that they’re the same as peptic ulcers which is not true.
Stress ulcer prophylaxis and current treatment for stress ulcer are reassuring in preventing clinically critical bleeding from the upper gastrointestinal tract, especially among severely ill patients who cannot take NSAIDs or anticoagulants due to their medical condition.
The critical point here is that while one can’t prevent all cases of severe illness, there are steps we can take to help reduce risk for stress, effects of stress and physical illnesses to better protect ourselves against life-threatening complications such as stress ulcers.